





General A case Report of Acute Myeloid Leukemia
2019.12.31 13:30
|
A case report of an Acute Myeloid Leukemia
History: A 71 years old Korean female (O.J. Kim) met her family MD for a "Once-a-year" medical check. She had no significant past medical history or any significant medical problems. On 9-30-2019 at the office, everything checked out well except: CBC shows WBC=1.7 with an Absolute Neutrophile Count of 0.4 (marked as critical). The red cell was slightly macrocytic. Otherwise, all other cell counts were normal. (This report only became available after her departure to an out-of-country trip.)
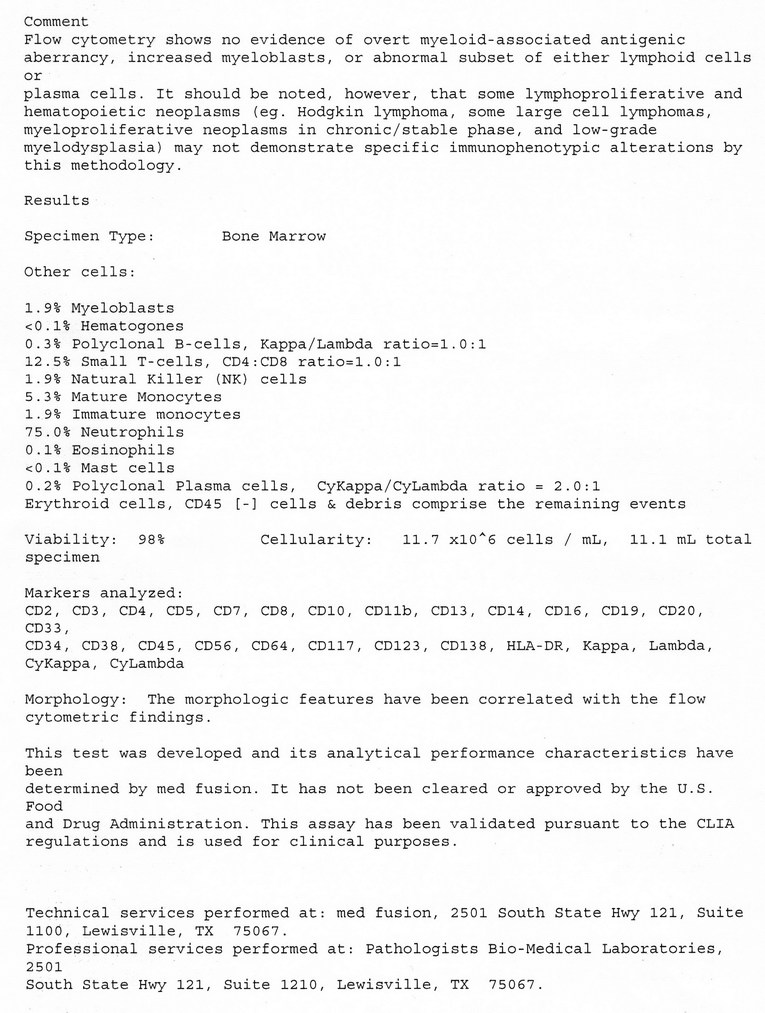
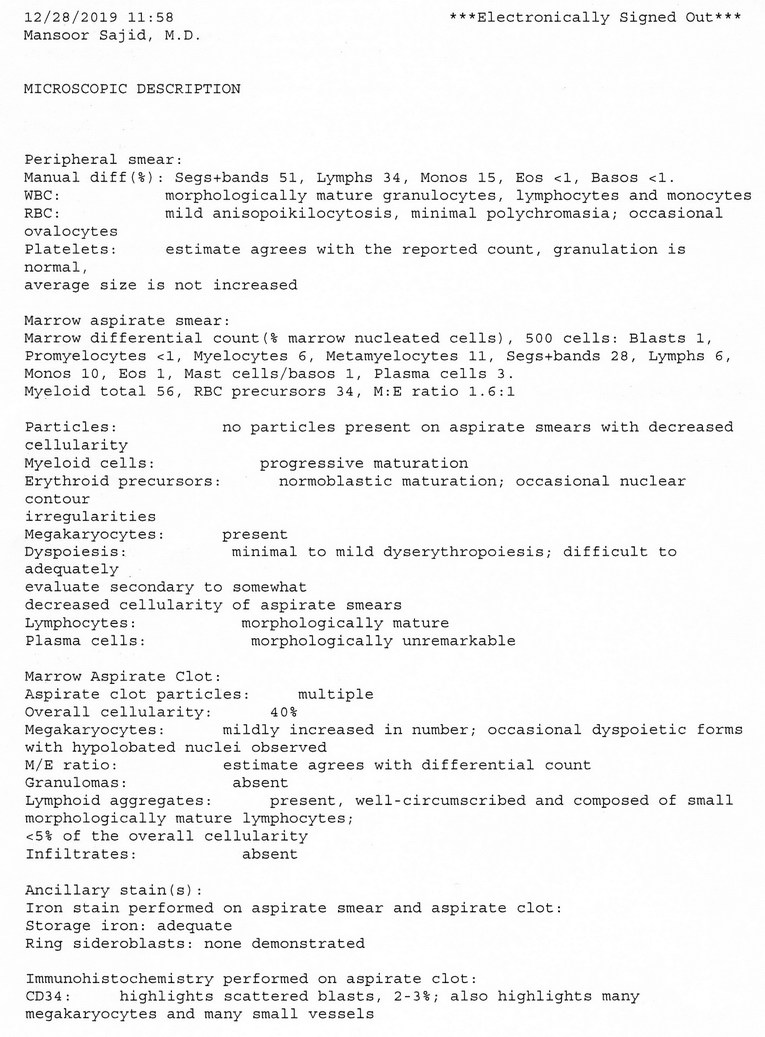
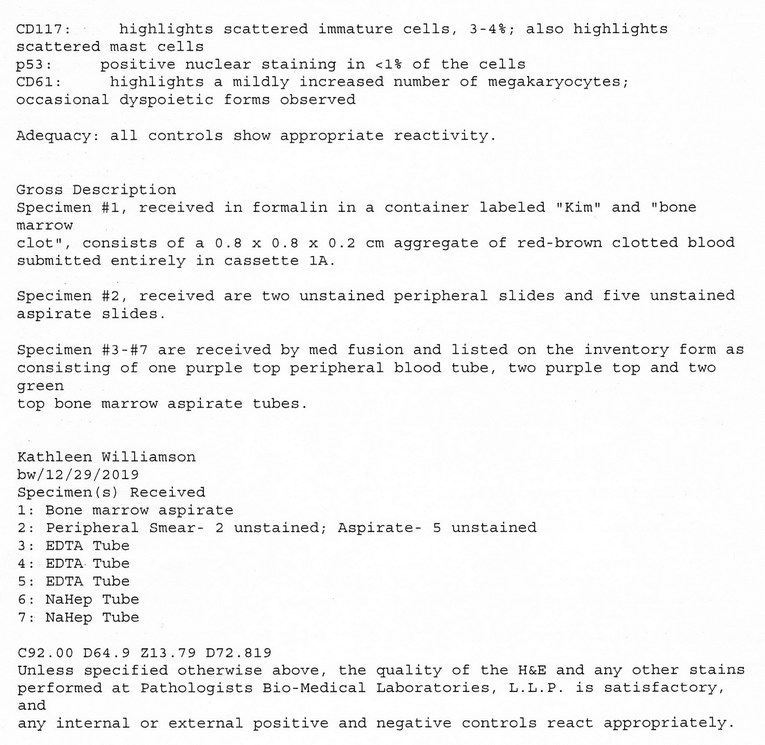
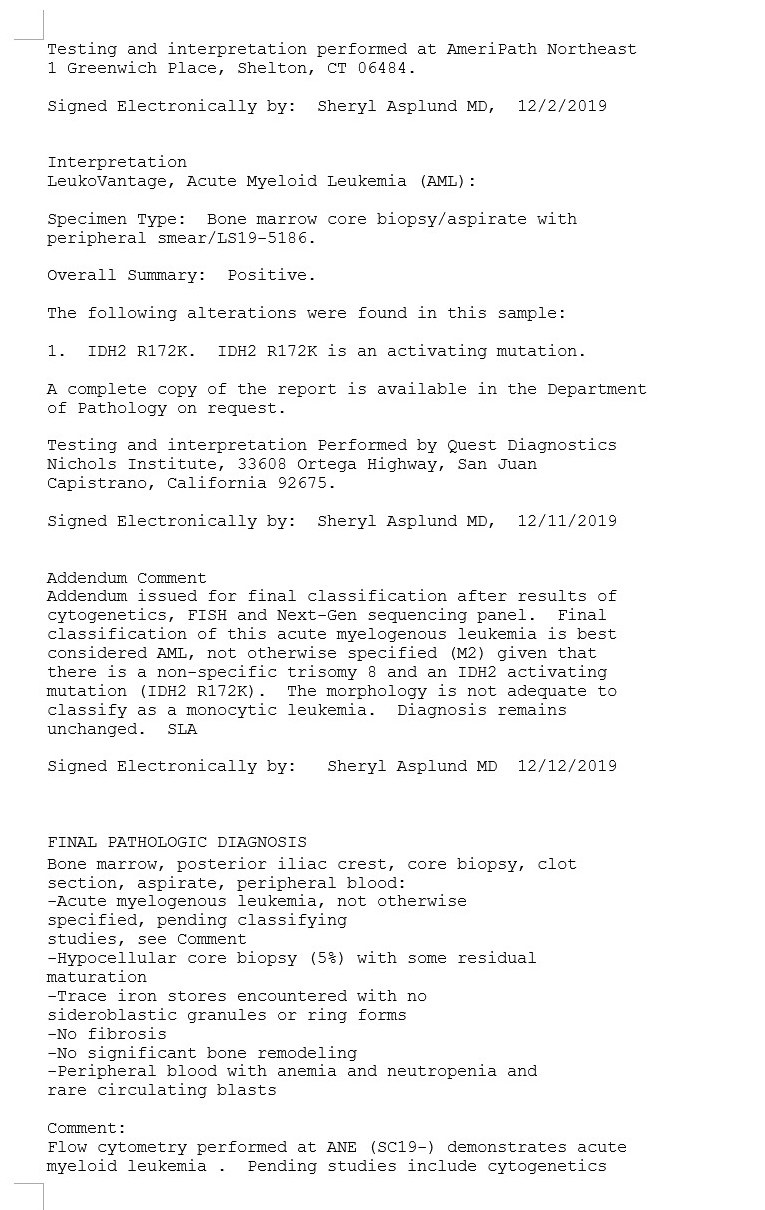
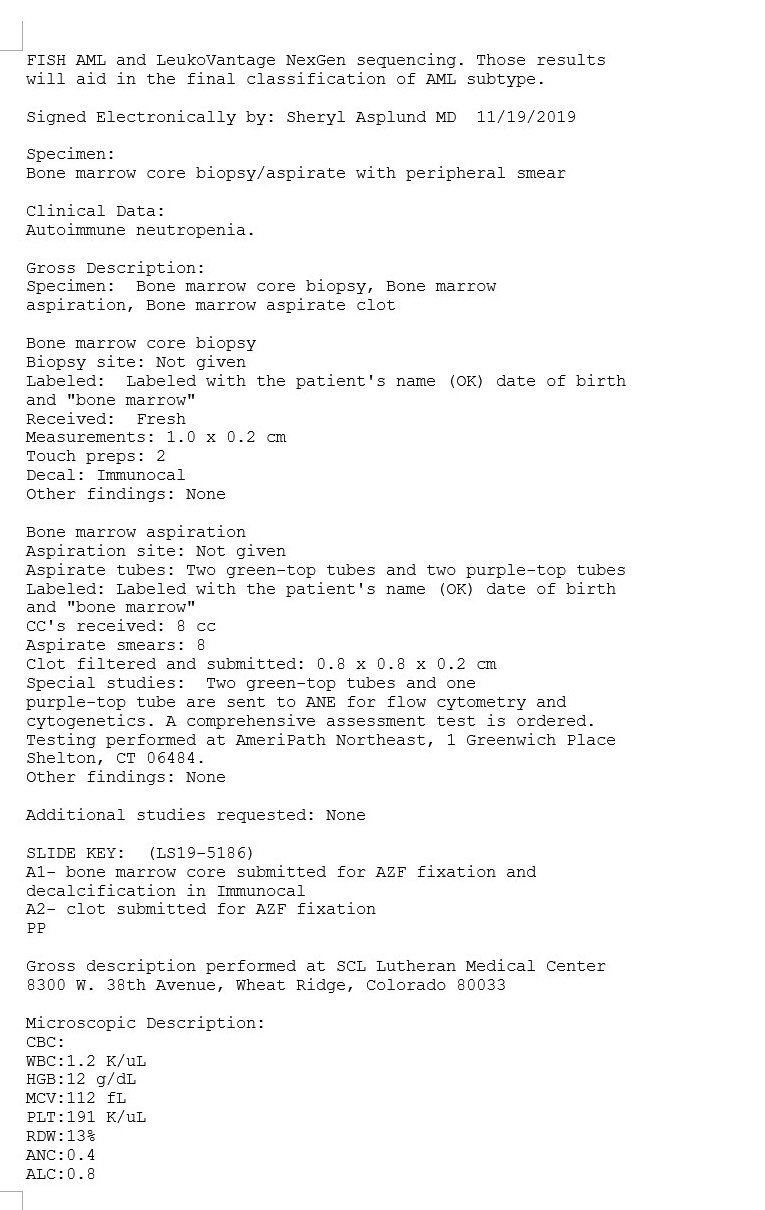
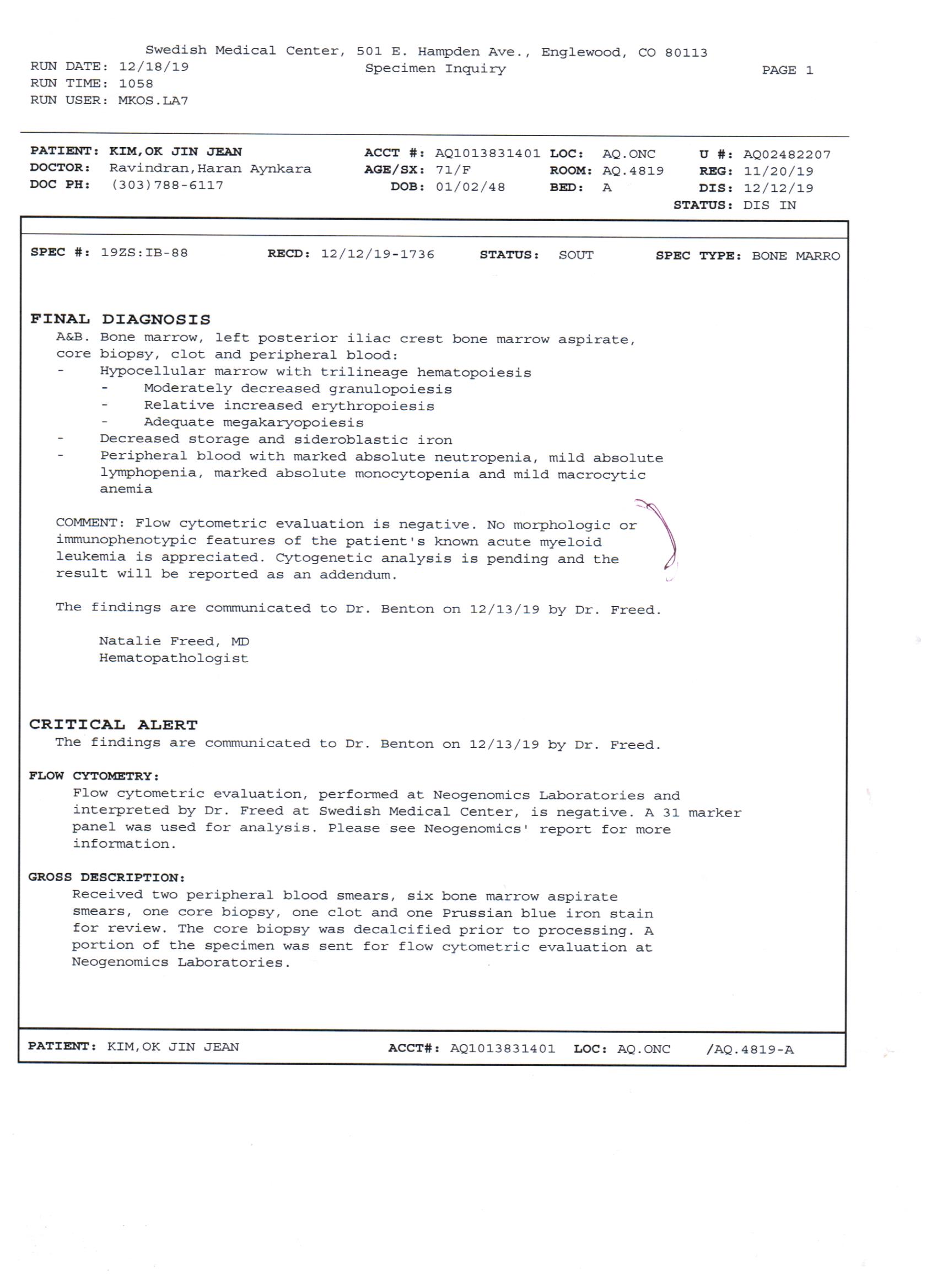
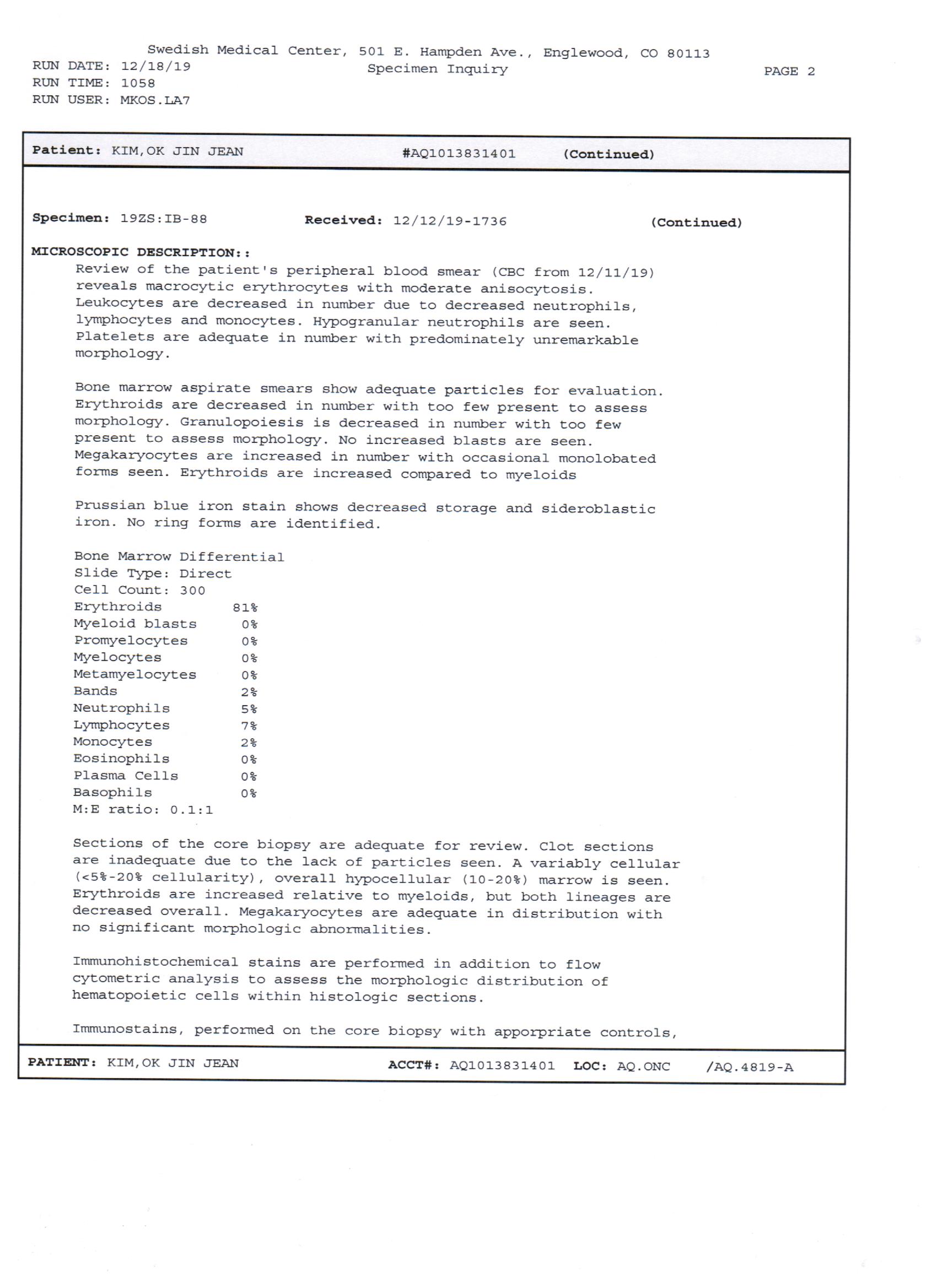
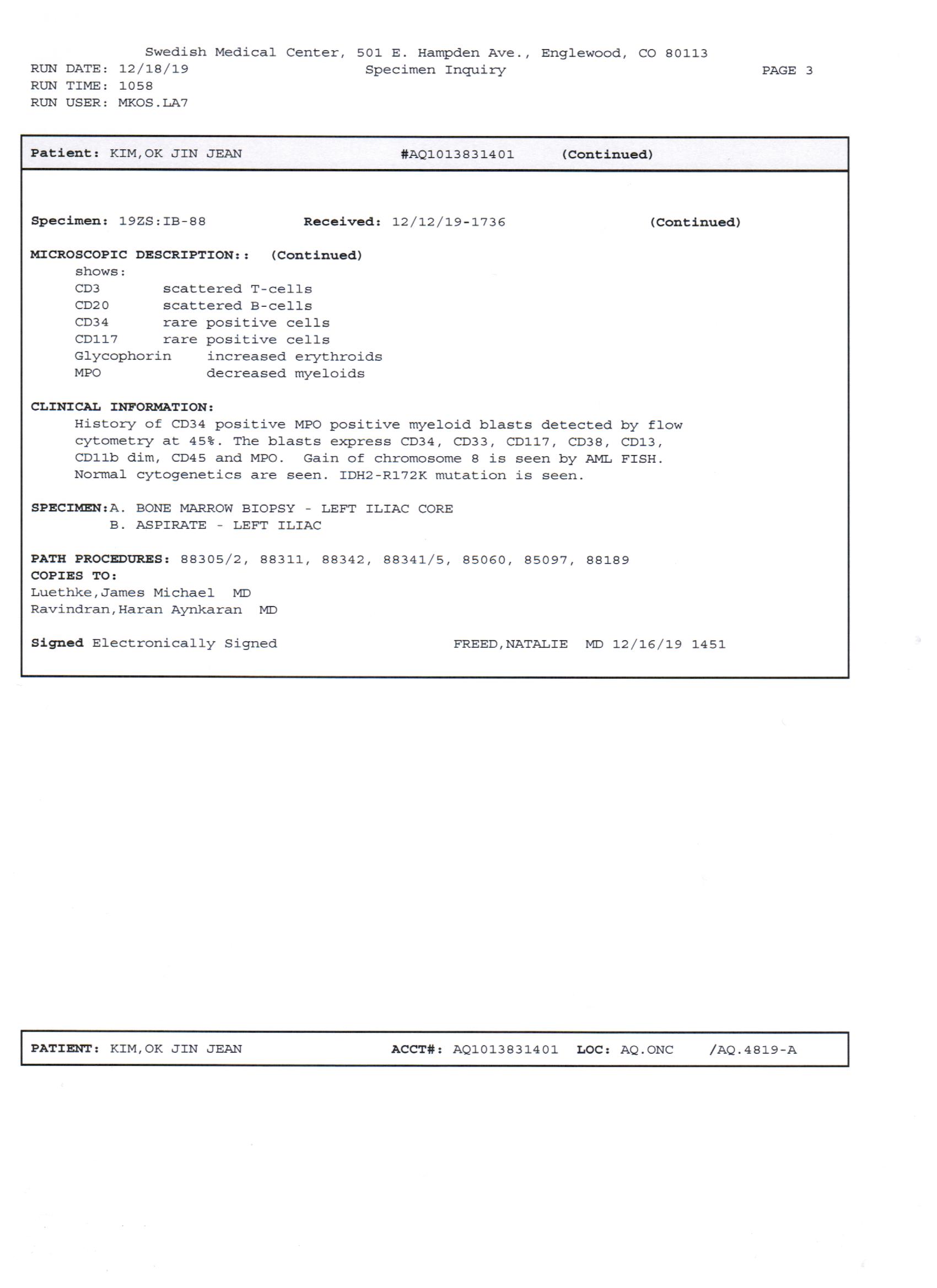
She returned from the trip 10-12-2019. She immediately revisited her MD on 10-13-2019 and took a retest of CBC. On that day, WBC=1.2, Absolute Neutrophil Count=N.A. She was referred to an oncology office on 11-14-2019. There, WBC=1.2, ANC=N.A. "Office" Bone marrow biopsy on 11-14-2019 showed increased blast cells with a diagnosis of possible Myelodysplasia. But the specimen was not sufficient enough for a definite diagnosis. She was referred to a hospital for better bone marrow biopsy. 11-18-2019: Bone Marrow block biopsy was read as a definite diagnosis of Acute Myeloid Leukemia. The following is the path report:
On the diagnosis of AML, she was admitted to Swedish Hospital the next day.
Chemotherapy and prophylactic antibiotic therapy were started on 10-22-2019 with: 1. Decitabine IV 30mg/day x 5days (original plan was for 7 days but it was shortened by the oncologist due to her satisfactory clinical course.) 2. Venetoclax P.O. 100mg/day concomitantly for 14 days. (due to antifungal prophylactic antibiotics, the usual dose of 400mg was reduced to 100mg) 3. Prophylactic Antibiotics and other drugs of : a. Apixaban (Eliquis) 5mg PO twice a day b. Levofloxacin (Levaquin) 500mg PO daily c. Valacyclovir (Valtrex) 500mg PO daily d. Voriconazole (Vfend) 200mg PO twice a day e. She received subcutaneous blood thinner (heparin?) daily.
The path report of the above bone marrow biopsy came a few days later. Our doctor noticed the mutation type of "IDH2 R172K" (above report) and said it was good that our medication so far was fitting to the particular situation well.
During the admission, daily blood count was done. The Absolute Neutrophil Count was as low as 0.8 and then gradually increased to 1.2 at the time of discharge. Hemoglobin dropped to as low as 9 but recovered to 11 at discharge without transfusion. Other blood cell counts (platelets and etc.) returned to almost normal by the time of discharge. She had no significant side reaction to the chemotherapy except below.
On 12-11-2019, one day before the discharge, she developed atrial fibrillation with a rapid rate. She was given Metoprolol Tart (Lopressor)12.5mg twice a day and it disappeared the next day. The family MD told her to stay on Metoprolol and she is still on it even today. She never had past history of any heart conditions or atrial fibrillation before, and the atrial fibrillation never recurred again so far after this episode.
She was given a prescription for all the above "5" medications on discharge.
Another bone Marrow Biopsy was done just before the discharge on 12-12-2019. The path. report on this biopsy is below.
At home, she did well with no particular symptoms or atrial fibrillations. 1. There were occasional nose bleeding of minor nature almost daily. She used to have those before. 2. She had a lip blister at about 12-23 to 12-25-2019 but healed spontaneously. 3. She had an episode of somewhat severe generalized body and bone aches (esp. knees) for 3-4 days at about 12-26-2019 and disappeared. Slight general weakness was felt only for a few days This was treated with Tylenol and Claritin and disappeared in a few days.
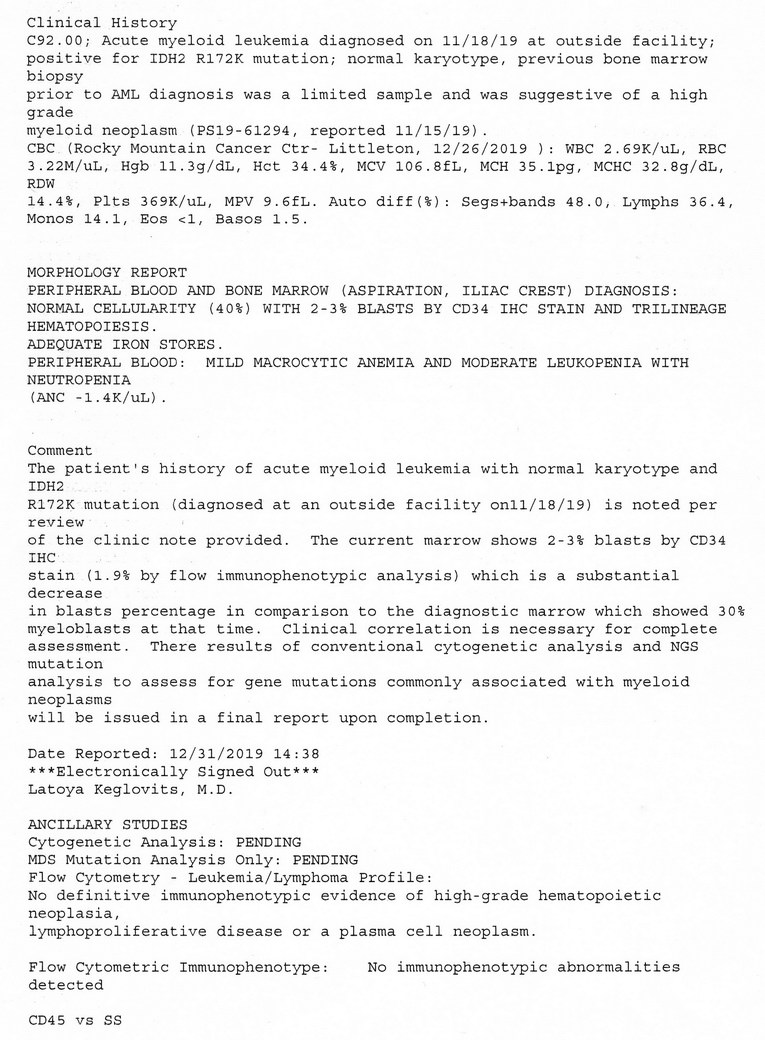
She visited her doctor on 12-26-2019 and had CBC and Bone Marrow Aspiration. There, her WBC=2.69, ANC=1.29. Bone marrow Aspiration reports below. (became available on 1-02-2020)
Without the above Bone Marrow Biopsy report, she was started on the "Second" Chemotherapy Plan of pre-planned "once a month" schedule starting from 12-30-2019. She was continuing all the prophylactic antibiotics and started on the same regimen of: 1. Outpatient IV infusion of Decitabine 30mg once daily for 5days 2. Combination therapy with Venetoclax 100mg PO daily for 14 days. She has no side reactions so far. Some anorexia, Possible general weakness and poss. mental depression that could have been from Metoprolol (Lopressor) or chemotherapy (?)
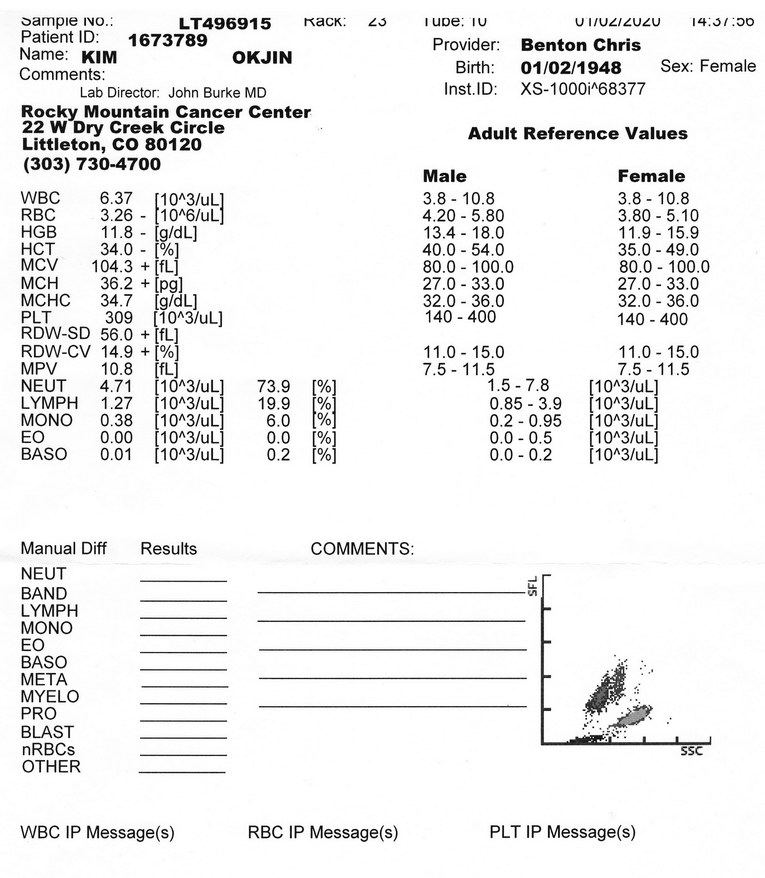
A CBC was done after the second day (1-02-2019) of IV Decitabine (x5days) combined with oral Venetoclax (x14days). The results are below.
She now faces two more days of IV Decitabine and 11 more days of Oral Venetoclax. She is to see the oncologist on 1-09-2020.
Report prepared by S. Steven Kim, M.D. FACS (husband, retired) on 1-03-2020 |
Comment 4
-
This report was made to send the information to two doctors specializing in leukemia
as an informal consultation. I thought sending the clinical history in the form of webpage
would be convenient for the doctors to see.
Our oncologist explained atrial fibrillation as possible cancer cell infiltration to atrium.
However, atrial fibrillation stopped the next day and has never recurred since.
Doc, thanks for your comments.
-
황규정*65
2020.03.02 23:04
Hi Steven!
Thanks for putting this medical information on our websites for us to read it.
It seems to respond well to chemotherapies to even eyes of plain a retired doctor
like me. We all happy for you and your family.We will pray continuously for her full recovery. -Jungsun and Kyu Jeong
-
Thanks. She's been doing well. Now, she's on maintenance chemotherapy once a month.
She goes into neutropenia after the chemo and then recovers quickly.
So, she has non-neutropenia days of about a week in a month between the chemo.
In the neutropenic period, we both go into isolation, less strict than the Coronavirus event.
For the time being, this is very restricting for an active couple like us.
But we, both, are in this together. Yes, the old age...
We came a long way and just got over a hill. And, there, we are looking at the setting sun.


HI Steven,
Thank you for sharing the detailed medical information on Ok Jin cee whom
all of her friends including Suk Joo and myself deeply care about like a member
of an extended family and constantly think about.
Just now belatedly I happened to take notice of your case report and quickly read it through.
Certainly, I was happy to have learned the favorable response she showed to the treatment so far.
Although much of the hematology report was beyond my scope of knowledge, I was puzzled
as you were why she experienced the episode of paroxysmal AF, which was well managed.
It is conceivable that the transient anemia with or without labile systolic hypertension in an
elderly patient could bring on PAF. I have seen it happening in a good number of elderly patients
I got involved with as a cardiologist. If that is the case, which I suspect it may be, the AF may not
recur as long as the anemia remains corrected. That is the only thing medical I could comment on.
Suk Joo and I will always think of Ok Jin cee and you, and you two will be in our daily prayer.
Lee, Hahn Joong